College of Respiratory
Therapists of Ontario
RESPONSIBILITIES UNDER
CONSENT LEGISLATION
Professional Practice Guideline
April 2022
PROFESSIONAL PRACTICE GUIDELINE
College of Respiratory Therapists of Ontario (CRTO) publications contain practice parameters and standards that should be considered by all Ontario Respiratory Therapists in the care of their patients/clients and in the practice of the profession. CRTO publications are developed in consultation with professional practice leaders and describe current professional expectations. It is important to note that these CRTO publications may be used by the CRTO or other bodies in determining whether appropriate standards of practice and professional responsibilities have been maintained.
Resources and references are hyperlinked to the Internet for convenience and referenced to encourage exploration of information related to individual areas of practice and/or interests. Bolded terms are defined in the Glossary.
It is important to note that employers may have policies related to an RT’s ability to obtain consent from patients/clients. If an employer’s policies are more restrictive than the CRTO’s expectations, the RT must abide by the employer’s policies. Where an employer’s policies are more permissive than the expectations of the CRTO, the RT must adhere to the expectations of the CRTO.
Obtaining consent to treat a patient is embedded within the CRTO’s standards of practice, in other words, it would be professional misconduct to proceed to treat a patient without consent. The CRTO’s Standards of Practice and A Commitment to Ethical Practice documents provide further guidance to RTs surrounding their obligation and accountability in obtaining consent. This Professional Practice Guideline (PPG) provides an overview of the legislation, specifically the Health Care Consent Act (HCCA) and Substitute Decision Act (SDA) for RTs. The information is structured to first describe how to obtain consent for treatment from a capable person, and then how to proceed with obtaining consent for an incapable person. The key terms in bold are defined in the Glossary.
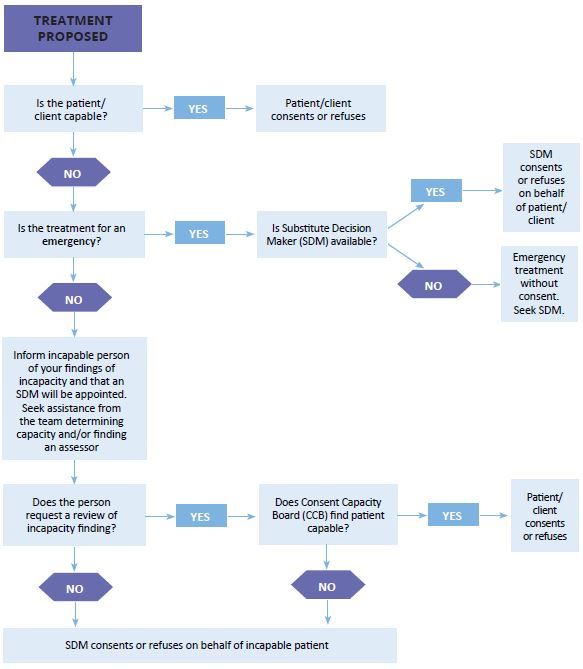
Obtaining consent can be guided by a step-by-step process that RTs should consider every time they are faced with obtaining consent for treatment. A decision tree is included as a visual aid below to assist RTs in their process of obtaining consent and to complement the outline of the PPG. RTs must remember to act within their scope of practice and use their professional judgement to always advocate for the best interests of their patients and assist patients/clients to understand the information relevant to making decisions to the extent permitted by the patients/clients’ capacity.
QUESTIONS OR FEEDBACK?
This Professional Practice Guideline will be updated as new evidence emerges or as practice evolves. Comments on this guideline are welcome and should be addressed to:
College of Respiratory Therapists of Ontario, 90 Adelaide Street West, Suite 300, Toronto, Ontario M5H 3V9
Phone 416-591-7800 | Toll Free 1-800-261-0528 | Fax 416-591-7890 | E-mail questions@crto.on.ca